Nandini Chatterjee, Dora Vargha, Rebecca Williams
University of Exeter
In a widely criticised interview with Sky News on 25 April 2021, the IT billionaire and philanthropist Bill Gates Jr. responded to a question whether he supported sharing the ‘recipe’ of the Sars-COV-2 or Covid-19 vaccines with manufacturers worldwide, with an emphatic: ‘No.’ No, he said, because there ‘are only so many vaccine factories in the world, and people are very serious about the safety of vaccines.’ Moving the production of a vaccine from Johnson and Johnson’s to a factory in India was already novel, he said, and could only happen because of ‘our grants and our expertise.’ Intellectual property was not holding back anything in this case, he said, because it wasn’t as if there were ‘idle vaccine factories with regulatory approvals, that make magically safe vaccines.’
It would appear from this account that most of the world was a place empty of funds and expertise, waiting for the largesse of saviours such as Bill Gates Jr. and appropriate guidance to be able to protect their own health in a scientific and safe way. Looking at the story of the Oxford-AstraZeneca vaccine with some more attention, however, produces some rather more complicated stories.
On 23 November 2020, an Oxford University-based research team led by Dr Andrew Pollard declared a breakthrough in developing an effective vaccine against Covid-19. The team had been working furiously for months, backed with UK government funding and public donations. Oxford University then announced a permissive protocol for licensing COVID-19 related IP to third parties under ‘these exceptional circumstances.’ Of the 5 points of guidance offered to organisations seeking licences to use Oxford University’s IP (or recipe for vaccine), one was: ‘The default approach of the University and OUI regarding (1) will be to offer non-exclusive, royalty-free licences to support free of charge, at-cost or cost + limited margin supply as appropriate, and only for the duration of the pandemic, as defined by the WHO.’
Such an approach is not unprecedented. In the 1950s polio epidemics swept through the globe, and in the midst of outbreaks two rivaling vaccines were developed by Jonas Salk and Albert Sabin, both without patent. When asked about this, Jonas Salk famously remarked ‘Would you patent the sun?’. It seems that the decision for the Salk vaccines lack of patent might have been a practical one, as it would not have been possible by contemporary standards, regardless of Salk’s moral stance. Sabin’s decision was an openly political one: the vaccine was a result of international collaboration between researchers of the two opposing sides of the Cold War, and this scientific exchange was greatly celebrated at the time. Of course, Gates is right that a lack of patent doesn’t automatically mean immediate access and capability of vaccine production everywhere in the world. It took years for many countries, in war-ravaged European states, up to half a decade to establish infrastructure, skill and procure materials (including live animals) for domestic vaccine productions of the Salk vaccine. However, many others had the capability, while standards of production were developed by the WHO, and this, in the end, dampened the dire global vaccine shortage in both the short and long run. More importantly, the lack of patent did not hinder national or global vaccination efforts.
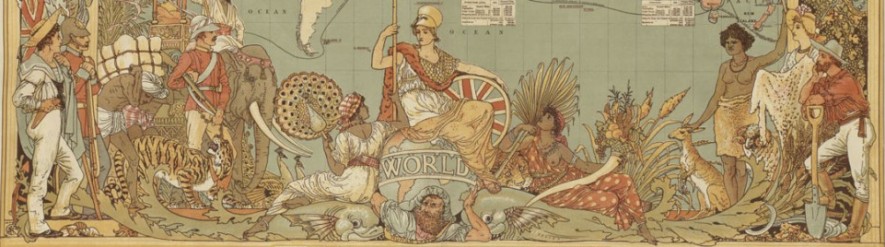
This permissive, humane approach, whereby human knowledge is shared freely for global human health, at least during the time of global danger from which no one is safe, was also proposed by the Oxford team. But it was soon lost to what is familiar to historians of colonialism as the ‘white saviour syndrome’. Urged, among others, by the Bill and Melinda Gates Foundation, Oxford University reversed its course, selling the knowhow of this life-saving vaccine, the cheapest of all vaccines around the world, to the pharmaceutical company AstraZeneca. The deal was exclusive, which means that the pharmaceutical giant now had sole rights worldwide and offered no guarantee of low prices. The revenues earned by Oxford University in this deal are unknown. In turn, AstraZeneca signed a deal with the Serum Institute, a private commercial pharmaceutical manufacturing company based in India. And finally, the Serum Institute agreed to supply the non-governmental organisation GAVI, previously called the Global Alliance for Vaccines and Immunisation, spearheaded and led by Bill and Melinda Gates Foundation, for its COVAX programme of supplying vaccines to the global south. The sacred circle was complete. The world would be saved by white saviours, as had been the case during the centuries of European colonialism (Vaughan, 1991), and as an added benefit, channel public funds into the private sector.
The narrative that is peddled is often exactly the opposite, however. Vaccines, just like any other drug, are hideously expensive to develop. For example, the average Research and Development spend between 1997-2011 by AstraZeneca per every drug approved was declared to be $12 billion dollars although such claims are disputed, hard to verify and often lowered by government subsidies. The most important component of these costs are those of the clinical trials, and this is where corporate funding usually comes in – no single research unit ever has the funds required to undertake the mass trials that are needed to make a drug safe. In this case, AstraZeneca spent a great deal of the money needed at the research end (the proportion appears impossible to establish). To speed up the process of production, the private Indian company called Serum Institute was given risk-free funds by the Bill and Melinda Gates Foundation, on the assurance that if the drug was not approved by regulatory approvals after all, Serum would not face any losses. It was all supposed to be win-win. Rather than assist unwieldy governments in the global south to produce their own essential drugs, ‘capitalist philanthropy’ would save the world.
Except it hasn’t. In the past two weeks, with a terrifying second wave of infections devastating India, the right-wing majoritarian BJP-led government of India, which, after irresponsibly relaxing all rational safety measures, has in the face of an impending humanitarian crisis, banned all export of vaccines, including from the Serum Institute – the main supplier of vaccines for the Covax programme. While some news channels in the UK have been shamelessly bleating at such vaccine nationalism – nearly 60% of UK’s 18+ population has received at least one dose of the vaccine, and less than 10% of India’s – the failure of this key supplier for GAVI means that the poorest countries in the world, many of them in sub-Saharan Africa, will not receive any doses at all until an unknown future. Dr. John Nkengasong, director of the Africa Centres for Disease Control and Prevention, has lamented that less than 1% of vaccines used in Africa, a continent of 1.2 billion people, are manufactured on the continent.
So, was Bill Gates Jr. right? That there was no technical and manufacturing capacity anywhere in the world – other than the profit-making Serum Institute owned by his chosen Indian capitalist, blessed by GAVI – with which the Oxford ‘recipe’ could have been safely shared? India has large installed capacity, even if not sufficient to entirely rule out the need for vaccine imports. As we have seen, together with South Africa, it had also put forward a proposal to the WHO for the waiving of patents, so one assumes Gates’ preferred corporate partner was not the only possible manufacturer. 9 other African countries also have some capacity.
The Serum Institute is the largest vaccine manufacturer in the world. But AstraZeneca’s vaccine, which it manufactures, is not the only COVID-19 vaccine around, nor is COVAX the only player even for the global south. Many other global supply structures are based on long-standing ties going back at least half a century, or reflect more recent geopolitical aspirations. Brazil, a country with high capacity for vaccine production is to manufacture a Russian-invented vaccine. China has been supplying rival vaccines around the world, prioritising export over domestic vaccination, often coupled with backdoor deals and paving the way for further investment. However, the fact that the current situation is dire for global vaccine access cannot possibly be overstated. It is part of a coordinated international effort that is much needed in a pandemic situation. The ways in which private interests, global power without accountability and humanitarian efforts intertwine in a crisis situation is devastating now, and worrying for the future.
Since at least the 1970s, scholars, activists and health professionals have been urging the need to ‘decolonise’ public health, among other things by widening global access to great inventions in therapeutics and moving beyond the patenting, marketing and pricing policies of pharmaceutical companies (Amrith, 2006; Greene, Condrau, Watkins, 2016; Rao, 1999)
When shall we #decolonise global health? Has the time still not arrived?
[Note to readers: This post is the first of a series on #DecolonisingPublicHealth which we will continue in the coming weeks.]
Further reading:
Sunil Amrith, Decolonising International Health: India and Southeast Asia, 1930-65 (Palgrave, 2006
J. Greene, F. Condrau and E. S. Watkins (eds) Therapeutic Revolutions: Pharmaceuticals and Social Change in the Twentieth Century (Chicago, 2016)
Mohan Rao, Disinvesting in Health: The World Bank’s Prescriptions for Health (New Delhi, 1999)
Dora Vargha, Polio Across the Iron Curtain: Hungary’s Cold War with an Epidemic (Cambridge, 2018)
Megan Vaughan, Curing their Ills: Colonial Power and African Illness (Stanford, 1991)


You must be logged in to post a comment.